Medical Research Funding: Impact on Patient Safety Oversight
Medical research funding plays a crucial role in advancing our understanding of health and safety, particularly for patients involved in clinical trials. With entities like the National Institutes of Health (NIH) providing significant grants, researchers can explore innovative treatments and therapies that ultimately improve patient care. However, recent funding cuts have raised concerns about the oversight and ethical treatment of participants, leading to heightened responsibilities for Institutional Review Boards (IRBs). These boards ensure that research adheres to health research ethics, prioritizing patient safety in research as a fundamental component of the process. Without adequate funding, the essential balance between innovation and ethical oversight may be compromised, potentially jeopardizing the very fabric of medical research.
Funding for health-related studies is essential for facilitating groundbreaking discoveries in patient care and safety. The financial support provided by governmental bodies, including the National Institutes of Health (NIH), underpins many clinical investigations that strive to uphold patient rights and welfare. The responsibilities assigned to oversight committees, such as IRBs, are central to maintaining ethical standards within these projects. By ensuring compliance with regulations and continuously monitoring participant safety, these boards are indispensable in the research landscape. A fall in financial resources could not only hinder innovative research but also risk the integrity of patient safety in trials across the nation.
Impact of Medical Research Funding on Patient Safety
Medical research funding plays a crucial role in ensuring the safety and ethical treatment of patients participating in studies. Without adequate resources, the operational capacities of Institutional Review Boards (IRBs) are critically weakened, which in turn jeopardizes patient safety. As research funding, especially from the National Institutes of Health (NIH), faces cuts, the ramifications for oversight are severe. These funds are essential for conducting thorough reviews of clinical trials, enabling IRBs to evaluate potential risks, assess informed consent processes, and ultimately safeguard the well-being of research subjects.
In the absence of robust funding, there is an increased risk of halting crucial studies that explore new treatments and interventions. In research environments where financial constraints abound, IRBs may struggle to maintain rigorous oversight. This compromises health research ethics and patient safety, leading to a loss of public trust in the medical research system. Proper funding is not just a fiscal matter; it is a moral issue that impacts how effectively medical research can protect those who bravely participate in clinical trials.
Understanding the Role of Institutional Review Boards (IRBs)
Institutional Review Boards (IRBs) are an indispensable part of the medical research landscape, tasked with protecting the rights and welfare of human research participants. Their responsibilities include reviewing research proposals for ethical considerations, ensuring informed consent is obtained appropriately, and continuously monitoring the safety of participants throughout the study. With the increasing complexity of clinical trials, especially those involving multiple sites, the importance of a single IRB system, supported by federal policies, becomes paramount in ensuring consistent oversight across various institutions.
IRBs are genuinely the ‘checks and balances’ that uphold the ethics needed in medical research. Their efforts not only scrutinize the risks and benefits associated with a study but also enhance the training and support provided to researchers. In situations where research funding is curtailed, the ability of IRBs to perform these critical functions may diminish, thereby amplifying risks to patient safety and the overall integrity of the research process. The continual evolution of research regulations, particularly following historical violations of patient trust, emphasizes the need for strong and well-funded IRB systems.
Consequences of Funding Cuts on Clinical Trials
The implications of funding cuts for clinical trials extend beyond immediate operational disruptions; they fundamentally threaten the trajectory of medical advancement. When research studies receive a stop-work order, as seen with the recent cuts to Harvard’s SMART IRB program, the ripple effects can delay critical investigations into groundbreaking therapies. With fewer resources available, research institutions may struggle to launch new studies or expand existing ones, ultimately stalling innovation. This disruption can diminish the enthusiasm of researchers and institutions, potentially leading to a decrease in the overall quality of biomedical research.
Moreover, with ongoing studies unable to recruit additional sites or participants, the information crucial for progress in treatment efficacy becomes stagnant. As patient safety in research is compromised—and public skepticism grows due to the visibility of funding issues—there is a tangible risk that communities will withdraw from participating in future studies. This withdrawal can create a feedback loop where diminished participation leads to reduced funding proposals, further hindering advancements in healthcare.
The Historical Context of Research Ethics
Understanding the historical context of research ethics illuminates the importance of robust oversight mechanisms like IRBs. The dark past of medical experimentation—highlighted by events such as the Tuskegee Syphilis Study and various unethical tests—underscores the necessity of ethical frameworks in modern research. These historical precedents have informed today’s oversight practices, aiming to protect human subjects from exploitation and harm. The evolution of research ethics has been a direct response to these egregious violations and acts as a reminder of the ethical responsibilities borne by researchers.
At the core of these historical lessons is the principle of informed consent and the ethical obligation to protect research participants. Today’s IRBs are a direct manifestation of society’s commitment to upholding these standards. Thus, any funding cuts that compromise these oversight bodies not only jeopardize patient safety but also erode the very foundation of trust that underpins clinical research. It’s paramount that funding mechanisms continue to support not just the pursuit of scientific knowledge, but also the ethical imperatives that keep participants safe.
Mobilizing Support for Research Ethics
In light of potential funding cuts, it is critical for the research community to mobilize public support for the ethical oversight of clinical trials. Engaging with stakeholders—including patients, healthcare providers, and policymakers—can help communicate the value of continued investment in research funding. By emphasizing the intersection between adequate funding and health research ethics, the community can advocate for the significance of protecting patient rights and safety. This involvement is vital as it illustrates how ethical research directly correlates with public health outcomes.
Moreover, fostering transparency about how funds are utilized within IRB systems can instill public confidence. Educating the community on the integral role that funding plays in maintaining ethical standards in research can further galvanize support. Highlighting the responsibilities of IRBs in ensuring patient safety reinforces the need for continuous funding to avoid regression in the ethical guidelines established to protect research participants in the first place.
Navigating Ethical Challenges in Collaborative Research
As medical research continues to trend towards collaborative models involving multiple institutions and sites, the ethical challenges become increasingly complex. This shift requires IRBs to adapt their oversight capabilities to ensure compliance with the more stringent requirements that collaborative research entails. With NIH funding being central to many collaborative initiatives, it is essential that these funds remain robust to support the administrative and procedural necessities of overseeing diverse research undertakings.
Navigating the intricacies of overseeing various sites also involves heightened responsibilities for IRBs, especially in the assessment and management of participant safety. Appropriate funding ensures these boards have the necessary resources to adequately monitor studies and address any unforeseen ethical dilemmas. As collaborative research becomes more prevalent, adequate funding emerges as a crucial element in sustaining the ethical infrastructure needed to protect human subjects across multiple study sites.
Strategies for Ensuring Patient Safety Amidst Budget Cuts
To mitigate the impacts of budget cuts on patient safety, innovative strategies must be employed by research institutions and IRBs alike. One approach is to enhance partnerships between academic institutions, community organizations, and funding bodies to foster a more resilient research infrastructure. By pooling resources and expertise, institutions can ensure that ethical oversight mechanisms remain effective even amid financial constraints.
Additionally, embracing technology can streamline administrative processes within IRBs, making them more efficient and cost-effective. Digital platforms for monitoring research compliance, managing informed consent, and conducting ethical reviews can help maintain oversight despite budgetary challenges. These advancements not only improve patient safety but also reinforce the commitment to uphold health research ethics, even in the face of potential funding disparities.
The Future of Medical Research Funding
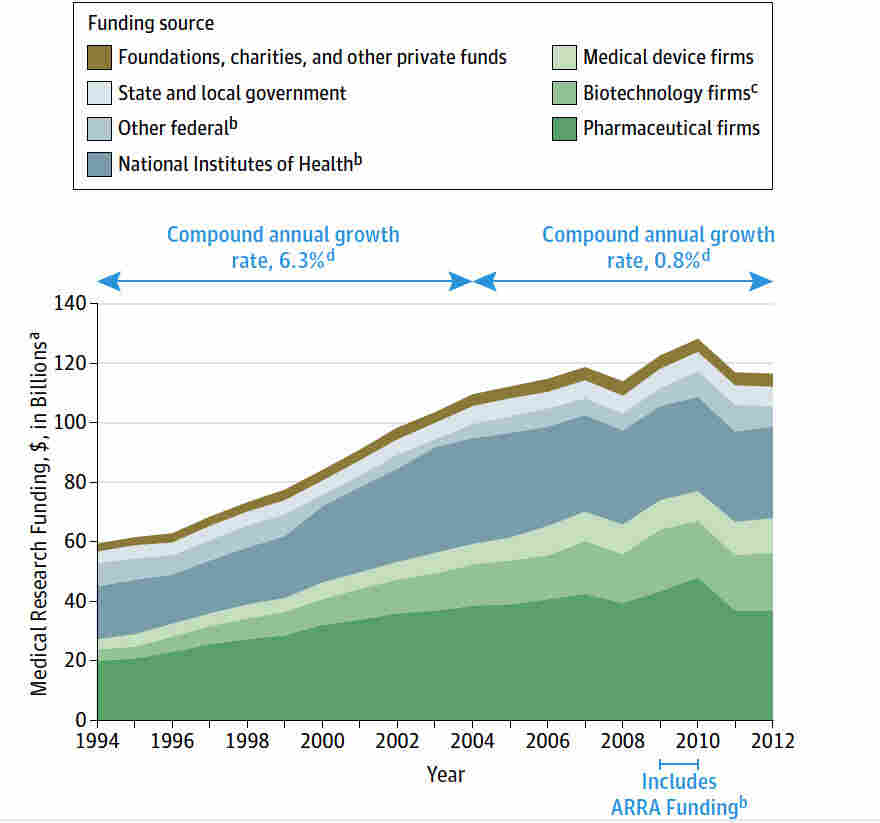
As we look to the future of medical research funding, it is crucial to advocate for robust financial support that emphasizes patient safety and ethical oversight. The ongoing debates surrounding funding allocations reflect broader societal values regarding healthcare and research. Engaging policymakers and the public in discussions about the critical need for sustained investment in research funding can help ensure that patient protection remains a priority.
Furthermore, diversifying funding sources can safeguard against the abrupt effects of federal budget cuts. Encouraging private sector involvement, philanthropic contributions, and community-based funding initiatives can create a more stable financial foundation for research. By promoting a shared responsibility for ethical medical research, this diverse funding landscape can strengthen the safety and rights of participants involved in clinical trials, thereby enhancing the integrity of the entire research enterprise.
Frequently Asked Questions
How does NIH funding contribute to patient safety in medical research?
NIH funding plays a crucial role in safeguarding patient safety in medical research by financing studies that are reviewed and overseen by institutional review boards (IRBs). These IRBs ensure that all research involving human participants adheres to established ethical standards and regulations, thereby protecting participants’ rights and well-being. Furthermore, NIH funding supports the necessary infrastructure for compliance, monitoring, and the repair of safety protocols during clinical trials.
What is the significance of IRB responsibilities in relation to medical research funding?
IRB responsibilities are integral to the context of medical research funding, as these boards oversee the ethical conduct of studies funded by NIH and other agencies. Properly funded IRB oversight ensures that research proposals are thoroughly evaluated for risks, benefits, and the ethical treatment of participants, which in turn helps maintain public trust in medical research and the effective allocation of funding.
How do funding shortfalls affect clinical trials oversight?
Funding shortfalls significantly impede clinical trials oversight by limiting the resources available to IRBs and research institutions. Without adequate funding, the capacity to conduct comprehensive reviews and ongoing monitoring is compromised, putting patient safety at risk. This can lead to halted or delayed studies, negatively impacting the integrity of medical research and the protection of participants.
What are the implications of medical research funding cuts on health research ethics?
Cuts to medical research funding have serious implications for health research ethics by undermining the operational effectiveness of IRBs. Such funding decreases the resources needed for ethical training, compliance reviews, and participant advocacy. Consequently, it may lead to lapses in ethical oversight, risking the safety, rights, and interests of participants in medical studies.
How can patient safety in research be compromised due to a lack of funding?
A lack of funding can compromise patient safety in research by hampering the ability of IRBs to carry out thorough evaluations of clinical trials. Insufficient funding results in fewer resources for monitoring adverse events, ensuring informed consent, and providing necessary training for research staff. These gaps may ultimately lead to increased risks for participants and a decline in the overall quality of research.
| Key Point | Details |
|---|---|
| Funding Freeze | The Trump administration froze $2 billion in federal research grants to Harvard, disrupting safety oversight in medical studies. |
| Impact on Patient Safety | The stoppage affects efforts to protect the rights and safety of patients involved in medical research. |
| Role of IRBs | Institutional Review Boards (IRBs) ensure compliance with regulations and protect patients by reviewing research proposals. |
| Historical Context | Past ethical violations in research led to the creation of IRBs to uphold participant safety and informed consent. |
| Consequences of Funding Cuts | Halting of studies, which risks patient safety, and exacerbates mistrust and skepticism in the research community. |
Summary
Medical research funding is critical for safeguarding patients in clinical studies. Recent funding freezes have put significant strain on oversight systems that ensure patient rights and safety. The implications of these cuts not only disrupt ongoing research efforts but also threaten public trust in the research community, ultimately jeopardizing the advancement of medical knowledge and innovation. It’s imperative that we recognize the importance of sustained investment in medical research funding to maintain the integrity and effectiveness of research practices.